We asked Dr. Jamie Chaves, a pediatric occupational therapist at The Center for Connection in Pasadena, California, to help us make sense of sensory processing. There is so much information out there - it can be hard to know what to ask and what to look for! We want to thank Dr. Chaves for helping us understand this complex issue.
---
Sensory input pervades our everyday lives. It is how we make sense of the world and interact with the world around us. It is how we learn new skills and participate in play, school, work, and self-care. We have 7 different sensory systems that our brain must integrate in order to interact appropriately with our environment. These sensory systems include: proprioception (muscle-joint awareness), vestibular (orientation in space), tactile (touch), auditory (sound), visual (sight), gustatory (taste), and olfactory (smell). Our brain works hard to integrate all of those sensations without becoming too overwhelmed, distracted, or disengaged.
Even things that don’t seem “sensory” actually are. Take handwriting, for example. In order to write, your brain must integrate a huge amount of sensory information: to remain upright in the chair (proprioceptive sense), to hold the pencil with an appropriate grasp using the appropriate force (tactile and proprioceptive senses), to form the letters appropriately with adequate spacing (visual and vestibular senses), to sustain endurance throughout the activity (vestibular and proprioceptive senses), to filter out distracting input (auditory senses).
Everybody processes sensory input differently and requires different amounts of sensory input to respond to the demands of the environment, maintain an appropriate level of engagement, and perform activities efficiently. Many of the ways we do this are functional and integrated into our everyday lives without second thought. For example, someone who is bored in a meeting might swivel her chair back and forth to help her pay attention better; someone who is nervous might calm her sensory system by chewing on gum.
Children (and adults) with sensory processing disorders (SPD) manage sensory input in ways that are not functional, meaning they interfere with their daily activities. For example, a child who is sensitive to tactile input may avoid wearing certain clothes, or a child who seeks tactile input might constantly touch people or objects around him. Thanks to University of California San Francisco (UCSF) researchers, we now have tangible evidence of differences in how neurotypical children process sensory input versus children with SPD. This is not behavioral—the behaviors are simply an outpouring of an attempt to do whatever necessary to get back to a regulated state.
An adaptive response occurs when a child can successfully overcome challenges or demands in the environment. This is only possible when the brain effectively organizes incoming sensory input. Many children with SPD do not have the tools necessary to attain an appropriate arousal level in their current environments or with their current self-regulation strategies—so they are too overstimulated or too understimulated. Many children with SPD also do not organize sensory input into meaningful information, so they require extra time to perform tasks, perform them inefficiently, or get frustrated easily.
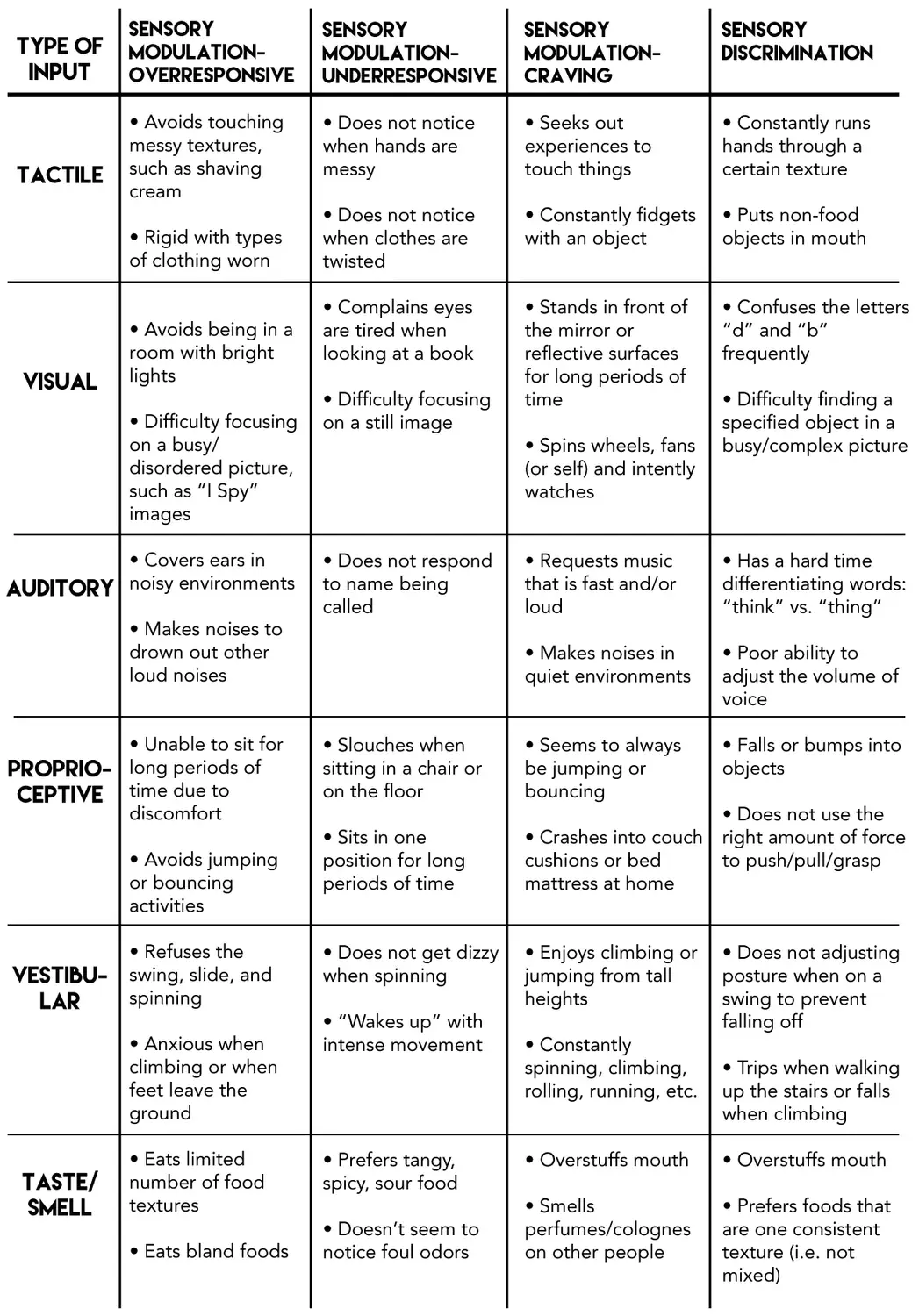
SPDs can manifest in different ways. The following table shows some of the possible different responses to sensory input. With Sensory Modulation Disorder, the brain processes either too much (overresponsive) or too little (underresponsive) sensory information. Children with Sensory Discrimination Disorder have difficulty telling the difference between sensory stimuli.
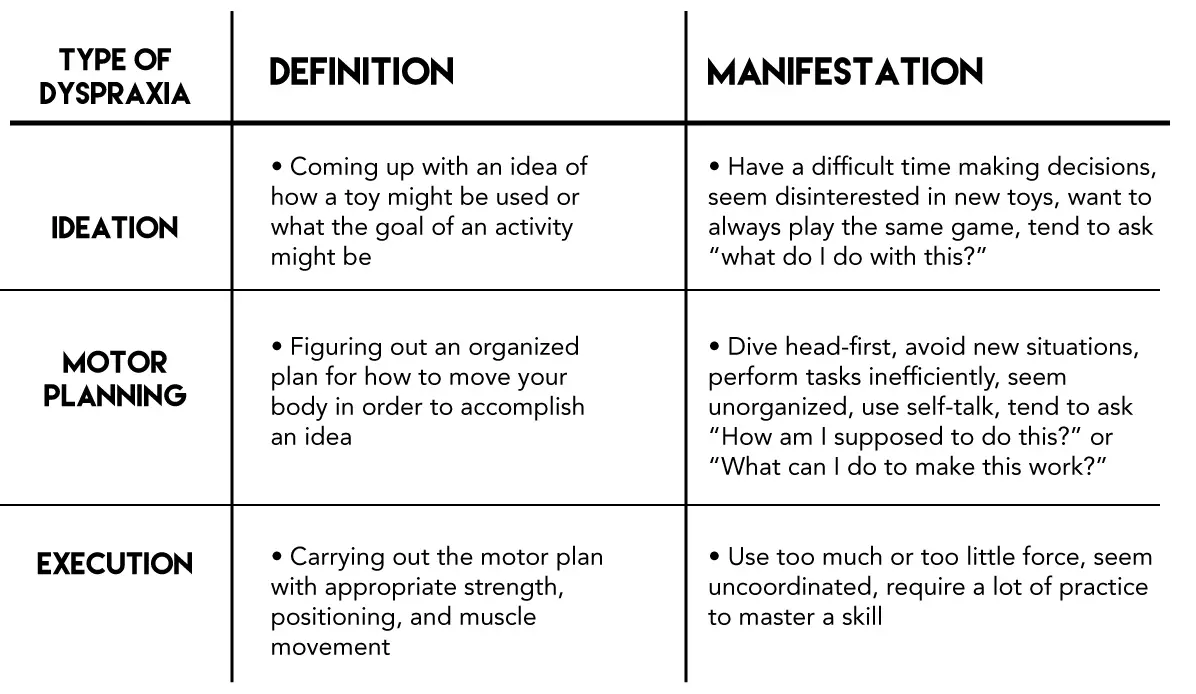
SPDs can also manifest in postural instability and dyspraxia—both of which are Sensory-Based Motor Disorders. Sensory-Based Motor Disorders occur when there is a disintegration of tactile, proprioceptive, and vestibular input. With postural instability, a child does not have the strength or endurance to sit upright without leaning on something (or someone), lying down, slouching, or changing positions. This inherently impacts the ability to focus at school or remain stable enough to write. Examples of dyspraxia are provided in the following table
SPD Support has a comprehensive online survey that can help further identify if a child has SPD. If a child has few, scattered challenges then a consultation with an occupational therapist might be helpful to identify strategies to address those areas of functioning. If a child has multiple challenges in one or more categories, then an evaluation with an occupational therapist is highly recommended. It is important to note that sensory processing concerns do not spontaneously arise—there is a developmental history to them. For example: an infant who was difficult to soothe, an infant who learned to crawl late (or never crawled at all), or an infant who refused to touch food on the tray. All are indicators of SPD. Research shows the following conditions have predisposition to SPD: prematurity, fetal alcohol syndrome, Autism, ADHD, fragile X syndrome, repeated ear infections, and sleep problems.
If, after you complete the SPD Support survey, you still believe the child has SPD, consider the following questions:
Does the child perform differently at school than at home or in the community? Recognize that some children “keep it together” at school but fall apart when they get home. Factoring in how a child functions in different environments is highly recommended.
After identifying that a child has or potentially has a SPD that is impacting his/her function and participation, many parents are not sure what the next steps should be. I encourage parents to seek an evaluation with an occupational therapist by either obtaining a referral from a pediatrician through their insurance or contacting a private practice occupational therapist. I always let the parents know that advocating for their child, even with the pediatrician, will be important. Many professionals still deny that SPD is a “real diagnosis” and still there are no ICD-10 codes for SPD.
I also encourage parents to pursue an IEP from their school district to see if school services can be provided. Some schools might provide services through a contracted outpatient clinic if they do not have the necessary equipment. Most children with SPD will also require services outside of the school setting.
Sensory integration works to change the neurological system in the brain so that the child processes sensory input more effectively. Over time, the more sensory input the brain receives in a therapeutic way, the better equipped the brain becomes to integrate all the sensory input from a variety of environments. While sensory integration helps to find a balance in the brain, the child will continue to need a variety of sensory outlets to help stay regulated—just like any well-organized adult. For example, the child might need to continue participating in swimming throughout the year, just as an adult may need to continue participating in yoga on a weekly basis. Because children have brains that are more plastic than adults, meaning they are still developing and the connections can be changed, the sooner SPD is recognized and services are pursued, the better the outcomes. It’s never too early but it’s never too late!
Dr. Jamie Chaves, OTD, OTR/L, SWC is a pediatric occupational therapist at The Center for Connection in Pasadena, CA. She also holds a California feeding and swallowing certification. The Center for Connection, founded by Dr. Tina Payne Bryson (author of and No Drama Discipline >th >is an interdisciplinary center that promotes health and happiness through a relationship-based perspective. For more information visit us online at: www.thecenterforconnection.org.
Share with
Related Resources